HOW MUCH VITAMIN D SHOULD I TAKE?
How Much Vitamin D Should I Take?
Vitamin D: Can You Have Too Much Of A Good Thing?
(Click on Nutritional Terms and Reference Numbers in Blue for More Info)
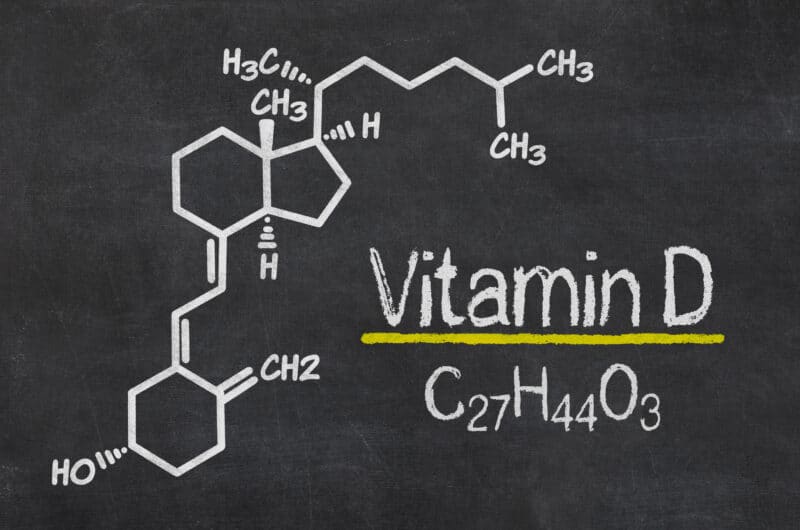
Vitamin D is a fat-soluble vitamin, which plays an essential role in many functions of the body necessary for good health and optimal performance. These include the regulation of phosphorus, maintaining the structure of bone and teeth, and normal immune function. It can help to reduce depression, aid weight loss and play a role in muscle growth and repair, cardiovascular exercise performance and recovery from exercise. It is particularly important for the intestinal absorption of calcium, magnesium, and phosphate, as well as many other physiological processes.
It’s role in immune function has received particular attention recently, as there are an increasing number of studies highlighting its role in the prevention and treatment of viral illnesses such as colds, flu and Covid 19.
In the last decade there has been a large increase in research into vitamin D, which has not only provided us with a better understanding of the vital physiological role it plays within the body but also the scale and effect of vitamin D deficiency, including among athletes.
For example, a review by Shuler et al., (1) noted in the US, that the incidence of vitamin D deficiency in elite indoor athletes is up to 94% of basketball players and 83% of gymnasts. It would seem reasonable to assume that participation in outdoor sports provides an advantage for vitamin D production. However, recent reports indicate otherwise. For example testing of the New York Giants (football players) during spring practise showed that 81% of players were deficient.
In the general population in the US, 50-70% of children and adolescents are deficient. Over 75% of whites and 90% of African Americans and Latinos are deficient, with increasing age increasing the likelihood of deficiency.
In addition, deficiency rates doubled between 1994 and 2004. Multiple factors are belived to be responsible for this increase, including sun avoidance, sunblock use, and increasing obesity rates, which reduce the availability of this fat-soluble vitamin in the body.
It is a similar situation in the UK, with low vitamin D levels commonly found in significant numbers of all population groups: in winter 30-40% of all age groups in the general population are classed as deficient. This figure has been shown to be as high as 93% in black and ethnic minority populations. Even towards the end of summer, 8% of adults and 13% of adolescents remain deficient. This has led many people to now include a vitamin D supplement as part of their regular nutrition strategy.
Despite deficiency being common, a story appeared in the media recently about a man who consumed an excessive amount of vitamin D, resulting in vitamin D intoxication, or hypervitaminosis D, a clinical condition characterised by elevated serum vitamin D3 levels.
This has caused something of stir, with many people understandably concerned that supplementing with vitamin D may be potentially harmful. So, in this article, we are going to look at the original case study published in the British Medical Journal (BMJ) (2), which is the source of the story, and explain what he did wrong and what we can do to avoid a similar fate.
Case Presentation
The case involves a middle-aged man who was referred to hospital by his family doctor after complaining of recurrent vomiting, nausea, abdominal pain, leg cramps, tinnitus (ringing in the ear), dry mouth, increased thirst, diarrhoea, and weight loss (28 lbs or 12.7 kg).
These symptoms had been present for nearly 3 months, and had started around 1 month after he began an intensive vitamin supplement regimen on the advice of a nutritional therapist.
The man had had various health issues, including tuberculosis, an inner ear tumour, a build-up of fluid in the brain (hydrocephalus), bacterial meningitis, and chronic sinusitis.
The results of blood tests ordered by his family doctor revealed that he had very high levels of calcium, slightly raised levels of magnesium, and his vitamin D level was 7 times over the level required for sufficiency.
Vitamin D – How Much Is Too Much?
The patient had been taking around 20 different nutritional supplements per day, the detailed discussion of all which is beyond the scope of this article. Most notably these included 150,000IU of vitamin D.
To put this in perspective, currently the NHS (Vitamin D – NHS (www.nhs.uk) recommends that children from the age of 1 year and adults need 400IU (10 micrograms) a day. This includes pregnant and breastfeeding women, and people at risk of vitamin D deficiency. However, the NHS suggests that you can take up to 4,000IU (100 micrograms) of vitamin D a day without adverse reactions. This applies to adults, including pregnant and breastfeeding women, the elderly, and children aged 11 to 17 years.
It is obvious that the patient’s vitamin intake was many times greater than recommended. However, it is important to note that although high dose supplementation can be detrimental and should be avoided unless medically supervised, in cases of severe deficiency, a doctor may prescribe much higher doses of vitamin D than those recommended for the general population.
Note: Time 4 Ultimate Vit-D provides you with 4000IU in two capsules. This allows you to adjust your intake according to your needs, and provides you with the maximum recommended dose if required.
How Much Vitamin D Should We Have In Our Blood?
The patient’s excessive vitamin D intake resulted in a blood level of >400nmol/L. Again, to put this in perspective a level of 75nmol/L (30ng/ml) is considered sufficient; while a level of >125nmol/L is linked to potential adverse effects, particularly at levels greater than 150nmol/L. Typically, vitamin D toxicity occurs when blood levels rise above 375nmol/L (150ng/ml) (2).
Interestingly, what is considered to be an optimal level of vitamin D is the matter of some debate. For example, although a vitamin D level of 75nmol/L is typically considered adequate, the Vitamin D Council recommends maintaining levels of 100–200nmol/L (40–80ng/ml and states that anything over 250nmol/l (100ng/ml) may be harmful.
In light of these recommendations, it is not surprising that with a blood vitamin D level of greater than 400 nmol/L, the patient experienced problems.
Typically, there are 6 main side effects of too much vitamin D. These are:
- Elevated blood levels
- Elevated blood calcium levels
- Nausea, vomiting, and poor appetite
- Stomach pain, constipation, or diarrhoea
- Bone loss
- Kidney failure
Other potential effects include drowsiness, confusion, apathy, psychosis, depression, stupor, and coma, hypertension and heart arrhythmias.
The authors of the case study noted that the manifestations of vitamin D intoxication, in terms of symptoms and signs, are largely due to the resultant effects of the high blood calcium levels, rather than vitamin D. This is because vitamin D increases calcium absorption in the gut.
Case Outcome
Once symptoms developed, the patient stopped taking his daily supplement cocktail, but the symptoms did not resolve.
He was admitted to hospital for 8 days, during which time he was given intravenous fluids to flush out his system and treated with bisphosphonates, drugs that are normally used to strengthen bones or lower excessive levels of calcium in the blood.
As vitamin D is stored in body fat and released into the bloodstream slowly, the effects of toxicity may last for several weeks or months after an individual stops taking supplements. Such was the case for the patient: two months after discharge from hospital, his vitamin D level was still abnormally high (>400 nmol/L), yet his calcium level had returned to normal.
In Closing….
While an excessively high vitamin D intake can be potentially harmful, the authors of the case study highlight the fact toxicity is uncommon. On the other hand, deficiency is commonplace, particularly at certain times of the year and amongst certain ethnic groups and can have a profoundly negative effect on both an individual’s health and performance. The subject of this case study consumed something like 37 times the recommend maximum amount. Consuming such massive amounts of any nutrient could be potentially harmful. For example, although water is essential for life, an excessive intake can result in a potentially fatal condition known as hyponatraemia, due to the resulting low levels of sodium in the blood.
The main lessons to be learnt from this case study are to always adhere to the guidelines of recognised authorities when taking supplements. If it is deemed necessary by a suitably qualified health care professional to consume levels above those generally recommended, the individual should be carefully monitored, which should include regular blood tests to ascertain the exact levels in the body and so avoid the dangers associated with abnormal levels. You can rest assured that if you are taking the recommended amount of vitamin D, you are highly unlikely to experience intoxication, but you will experience the many benefits provided by maintaining the appropriate levels. As the old saying goes: “Moderation in all things”.